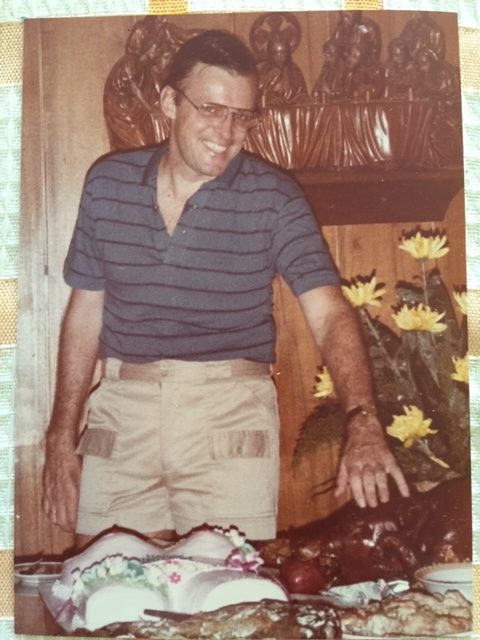
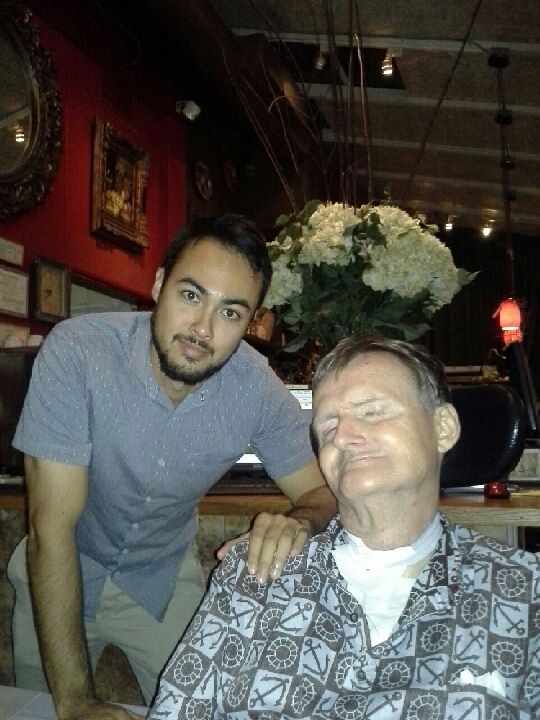
The following is an excerpt from Britt’s article, “Communication Problems in the Intensive Care Unit,” that was published in Qualitative Sociology, 1994, Vol. 17, No. 4, p.386. Britt spent three months in the Queen’s ICU for management of complications of a poorly managed pneumonia, which sent him back to the hospital ER in near respiratory failure. He was subsequently trached and vented. Although he was able to regain ability to breathe on his own after this hospital stay, he was fed through a gastrostomy tube for the rest of life. Britt passed away in 2015, four years after retiring from his faculty position at the University of Hawaii-Manoa. He preferred to have an assistant read his lips to dictate his manuscripts rather than use eye/gaze technology, which was still an early innovation in the 90’s. A human assistant, he said, guaranteed him social interaction every day at the office, at a time when his friends and colleagues stop calling on him in his office. Britt was truly a social scientist.
I found not having a real time voice was the equivalent to not having any defense to what was done to my body and once my body was touched, I had no control over the intensity or the painful effects of the procedure. I came to visualize having a voice as having a defense of making assertions about myself, making threats, and counter threats, and otherwise carving out and maintaining an interfactional space for myself. Not only could I not control what was happening to my body, I found I could not control the interactions which largely made up my person. I could not even communicate simple information about my condition to my doctors and most of my nurses. It was very difficult to gain people’s attention and maintain that attention through a course of conversation. The physicians, operating under tremendous subjective time pressures, would limit their visits to my room to fifteen minutes, time enough for only a few, if any, of my laboriously formatted sentences. The physicians would suggest that I formulate what I had to say before they came. This suggestion left out the possibility to respond to any emergent conversation while they were in the room. It also assumed that I would remember what I wanted to say in conversational contexts long after the conversation had passed. Some physicians made decisions in the room about treatment, including surgery, and I could not respond, besides giving a simple yes or no with head movements. If I wanted to enter a qualified answer, it was impossible, and many times the physician would leave the room while I was trying to spell out a reply. Often the physician would not see himself being addressed by my reply, the time lag was too great and his attention had switched to a new task, and the person interpreting what I was trying to say was so concerned about reading my lips or using my alphabet board that she or he forgot to signal the physician that I was saying something to him.
Not being able to conversationally influence most aspects of my experience in the hospital generated frustrations, resentments, and attributions about my intelligence, my motivations, and equally from my perspective, about the intelligence, motivations, sensitivity and the irrationality of the entire health care delivery system.